Alcohol withdrawal is a challenging journey that many individuals face when they decide to stop drinking. Understanding the alcohol withdrawal timeline can help prepare for this process, ensuring a safer and more comfortable experience. In this comprehensive guide, we’ll delve into the different stages of alcohol withdrawal, the factors that influence its progression, and the treatment options available to manage symptoms and maintain long-term sobriety.
Key Takeaways
- Alcohol withdrawal is a response to the disruption of neurotransmitter activity that occurs when ceasing or reducing alcohol consumption.
- Factors influencing the timeline of alcohol withdrawal include drinking habits, severity of dependence and personal health & medical history.
- Treatment options for managing symptoms are available, including medical detoxification, medications and supportive care/therapy. Relapse prevention includes building a support network and developing healthy coping mechanisms.
Understanding Alcohol Withdrawal

Alcohol withdrawal is a physiological and psychological response that occurs when someone with an alcohol use disorder ceases or drastically reduces their alcohol consumption. The cessation of alcohol intake disrupts the equilibrium between inhibitory and excitatory neurotransmitter activity, leading to a wide array of withdrawal symptoms.
These symptoms can range from mild discomfort to alcohol withdrawal seizures, depending on the individual’s level of alcohol dependence and other factors.
Alcohol Dependence and Withdrawal
Alcohol dependence, also known as alcohol addiction, is a condition in which an individual relies on alcohol both physically and psychologically, often leading to substance abuse, specifically alcohol abuse. According to the American Academy of Family Physicians, the stages of alcohol withdrawal can range from mild to more severe symptoms, depending on the level of physiological alcohol dependence.
Severe withdrawal symptoms may require immediate medical attention and can even be life-threatening.
Understanding the relationship between alcohol dependence and withdrawal is key. When someone with alcohol dependence stops drinking, their body must adapt to the absence of alcohol, leading to withdrawal symptoms. Factors such as the duration of alcohol use and the level of dependence can significantly influence the severity of withdrawal symptoms.
Fact: According to the latest statistics by National Institute on Alcohol Abuse and Alcoholism, in America, an estimated 88,000 people die from alcohol-related causes annually.
Causes of Alcohol Withdrawal
Prolonged and excessive alcohol consumption disrupts the balance between inhibitory and excitatory neurotransmitter activity in the brain. When an individual ceases or reduces their alcohol intake, this disruption leads to a hyper-aroused state and the onset of alcohol withdrawal symptoms, which may manifest within hours of the last drink.
Gamma aminobutyric acid (GABA) and glutamate are two neurochemicals associated with the development of alcohol withdrawal syndrome. Factors that contribute to the emergence of withdrawal symptoms include the level of alcohol dependence and the duration of alcohol use. Individuals with a history of heavy and chronic alcohol use may experience more severe withdrawal symptoms when they stop drinking.
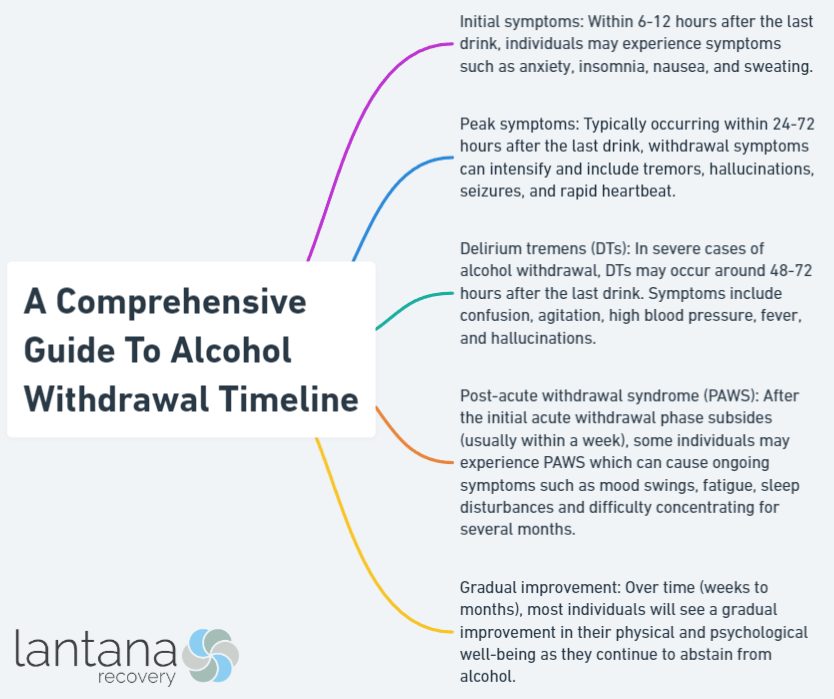
Alcohol Withdrawal Timeline: A Step-by-Step Breakdown

Physical withdrawal symptoms of alcohol usually reach their highest intensity between 48 and 72 hours after the last drink. They can last from 7 to 10 days, or even as long as 2 weeks. During the detox process, it’s beneficial to understand the timeline of alcohol withdrawal as it enables individuals and their support networks to better anticipate and handle symptoms.
The alcohol withdrawal timeline will be analyzed next, focusing on three distinct stages: initial symptoms, progression of symptoms, peak symptoms and delirium symptoms.
Initial Symptoms (6-12 hours)
Mild withdrawal symptoms typically commence within the first 6-12 hours after the last alcoholic beverage. During this initial stage, individuals may experience:
- Anxiety
- Irritability
- Nausea
- Vomiting
- Tremors
- Sweating
- Insomnia
- Restlessness
- Nervousness
- Pale or clammy skin
- Loss of appetite
Other mild symptoms may also be present.
Although these initial symptoms can be uncomfortable, they are relatively mild compared to the more severe symptoms that may follow in the next stage of the withdrawal process. Recognizing these early signs and seeking the necessary support is paramount for a safe and effective detoxification.
Progression of Symptoms (12-48 hours)
As the alcohol withdrawal process progresses, symptoms typically increase in severity during the 12-48 hour period after the last drink. Some common symptoms include:
- Tremors
- Sweating
- Nausea and vomiting
- Anxiety and restlessness
- Headache
- Insomnia
- Increased heart rate and blood pressure
Seizures and some milder manifestations like memory loss from alcohol withdrawal may be experienced during this time. Monitoring these symptoms closely is imperative, as rapid escalation may necessitate medical intervention.
Individuals experiencing this stage of alcohol withdrawal should be vigilant about their symptoms and seek medical attention if necessary. The role of professional support during this stage is pivotal as it can be the determining factor between a safe, successful detox and potentially dangerous complications.
Peak Symptoms and Delirium Tremens (48-72 hours)
The peak stage of alcohol withdrawal occurs between 48 to 72 hours after the last drink and can be the most dangerous phase of the process. During this time, individuals may experience:
- Nausea
- Vomiting
- Tremors
- Agitation
- Seizures
- Hallucinations
Severe symptoms, such as delirium symptoms, may also develop, requiring immediate medical attention.
Delirium tremens is a severe syndrome associated with dangerous complications, such as:
- Cardiac arrhythmia
- Respiratory arrest
- Oversedation
- Aspiration pneumonitis
These complications can be fatal or cause severe infections. Individuals with a history of alcohol withdrawal, extended periods of excessive alcohol consumption, or prior withdrawal seizures are at a heightened risk for developing delirium symptoms.
Seeking professional help and support from mental health services administration during this stage is crucial for symptom management and safety assurance.
According to a review study published in JAMA on the management of alcohol withdrawals, “Alcohol withdrawal delirium is the most serious manifestation of alcohol withdrawal and evidence suggests that appropriate care improves mortality.” (Management of Alcohol Withdrawal Delirium: An Evidence-Based Practice Guideline, Mayo-Smith et al., 2004)
Factors Influencing Alcohol Withdrawal Timeline

The timeline of alcohol withdrawal can vary for each individual, depending on factors such as:
- Age
- Gender
- Genetics
- Overall health
- Alcohol use history
Furthermore, the severity of alcohol dependence, the duration of alcohol use, and any underlying medical or psychiatric conditions can also influence the withdrawal timeline.
Identifying and addressing these factors can customize the detox process to meet the individual’s specific needs, leading to more effective treatment and long-term recovery outcomes.
Drinking Habits and Severity of Dependence
Drinking habits significantly impact the alcohol withdrawal timeline, with the frequency and quantity of alcohol consumed affecting the degree and duration of withdrawal symptoms. Heavy and extended drinking habits are likely to lead to more intense withdrawal symptoms and an extended withdrawal timeline, causing greater challenges during the detox process.
Alcohol dependence also plays a significant role in determining the intensity and duration of withdrawal symptoms. Those who are more dependent on alcohol are more likely to experience more pronounced withdrawal symptoms and a longer withdrawal timeline, emphasizing the need for personalized treatment approaches based on the individual’s unique circumstances.
Personal Health and Medical History
Personal health and medical history can significantly influence the alcohol withdrawal timeline. Individuals with inadequate overall health may experience more extended and more severe withdrawal symptoms, making the detox process even more challenging. Certain medical conditions or medications can also interact with alcohol withdrawal, potentially prolonging the timeline.
For a safe and effective detoxification, individuals are advised to consult a healthcare professional for a personal health evaluation and to create a secure and efficient withdrawal plan. This evaluation can help identify potential risks and complications, allowing for a more tailored and supportive detox experience.
Treatment Options for Managing Alcohol Withdrawal

There are various alcohol withdrawal treatment options available for managing alcohol withdrawal symptoms and ensuring a safe detox process. These options include medical detoxification, medications for alcohol withdrawal, and supportive care and therapy.
By exploring these treatment options, individuals can find the best approach to manage their withdrawal symptoms and transition into long-term recovery.
Medical Detoxification
Medical detoxification, or medical detox, is the process of safely managing withdrawal symptoms in individuals who have ceased using drugs or alcohol. This initial step in addiction treatment involves the use of medications and medical supervision to assist individuals in withdrawing from substances in a safe and comfortable manner. Medical detox is critical; it aids in minimizing the physical and psychological discomfort associated with withdrawal while enhancing the chances of successful recovery.
Those with moderate to severe symptoms of alcohol withdrawal require inpatient monitoring and treatment at an acute care hospital or detox-equipped facility. Those with a risk of exhibiting such symptoms should also seek this kind of specialized care. In severe cases, individuals experiencing intense symptoms or delirium symptoms may be admitted to a hospital ward or the intensive care unit (ICU) for medical attention.
Medications for Alcohol Withdrawal
Commonly prescribed medications for treating and preventing severe withdrawal symptoms include benzodiazepines, such as diazepam, chlordiazepoxide, and lorazepam. According to the chapter 4 of book Detoxification and Substance Abuse Treatment by SAMHSA, medications like Benzodiazepines can reduce intensity of withdrawal symptoms and prevent potential complications like Delirium Tremens, making the detox process more manageable for the individual.
In addition to benzodiazepines, other medications may be prescribed to address specific symptoms or complications arising during the withdrawal process. Working closely with medical professionals is crucial to determine the most suitable medications and treatment plan tailored to each individual’s unique needs and circumstances.
Supportive Care and Therapy

Providing supportive care during the withdrawal process is vital to ensuring the safety and comfort of the individual undergoing withdrawal. This care may include monitoring vital signs, ensuring adequate hydration and nutrition, and managing any symptoms or complications that may arise.
In addition to medical care, therapy and counseling play a vital role in the withdrawal process. By addressing the underlying causes of addiction and providing emotional support, therapy can help individuals develop the skills and coping mechanisms needed to maintain long-term sobriety. Various therapy options include:
- Individual counseling
- Group counseling
- Support groups
- Inpatient rehabilitation
These options offer valuable resources and guidance throughout the detox and recovery journey.
Preventing Relapse and Maintaining Sobriety

Prevention of relapse and maintenance of long-term sobriety after completing alcohol detox are fundamental for successful recovery. Strategies for preventing relapse include building a support network, developing healthy coping mechanisms, and participating in ongoing treatment and recovery programs.
By implementing these strategies, individuals can navigate the challenges of sobriety and lead fulfilling, alcohol-free lives.
For more information on how to effectively manage alcohol withdrawal at home, read our article on home remedies for alcohol withdrawal.
Building a Support Network
Establishment of a strong support network is key to maintaining sobriety. A support network consists of friends, family, and peers who can provide emotional and practical assistance during challenging times. This network can help reduce feelings of isolation and create a sense of belonging, making it easier to resist the temptation to return to alcohol use.
To build a robust support system, individuals should communicate with family and friends, participate in support groups, and consult with professionals. Being open and honest about one’s needs and being willing to accept help from others can significantly strengthen the support network and contribute to long-term sobriety.
Developing Healthy Coping Mechanisms
The need for healthy coping mechanisms becomes paramount when replacing alcohol use as a way of managing stress and emotions. These mechanisms can include:
- Obtaining adequate sleep
- Consuming a nutritious diet
- Engaging in regular physical activity
- Utilizing relaxation techniques such as deep breathing
- Constructing and upholding boundaries
To implement healthy coping mechanisms, individuals should:
- Begin by setting realistic goals and breaking them down into smaller, achievable steps.
- Prioritize self-care and take time for oneself.
- Seek support from friends, family, and professionals.
These coping mechanisms can contribute to long-term sobriety.
Ongoing Treatment and Recovery Programs
Continual treatment and recovery programs for alcohol withdrawal symptoms equip individuals with necessary tools and support to maintain long-term sobriety. These programs help individuals identify and confront triggers, develop healthy coping mechanisms, and establish a strong support network. By participating in these programs, individuals can continue to build upon the progress made during detox and maintain their sobriety.
Various pathways to recovery include:
- 12-step programs
- Faith-based programs
- Holistic approaches
- Alternative therapies
Each pathway offers different methods and approaches to recovery, allowing individuals to explore and find the most suitable option for them.
Aftercare support, such as individual and group therapy, support groups, and other resources, can provide ongoing support and guidance to help individuals stay on track with their recovery goals.
Summary
Navigating the alcohol withdrawal timeline can be a challenging and daunting process. However, understanding the stages of withdrawal, the factors that influence its progression, and the available treatment options can help individuals manage their withdrawal symptoms more effectively and achieve long-term sobriety. By building a strong support network, developing healthy coping mechanisms, and participating in ongoing treatment and recovery programs, individuals can successfully overcome the challenges of alcohol withdrawal and lead fulfilling, alcohol-free lives.
Frequently Asked Questions
How long after you quit drinking does your body return to normal?
It typically takes 3-4 weeks for the body to return to normal after quitting drinking. At 3 weeks, most drinkers will have reduced their risk of heart disease, improved kidney health and vision, and dependent drinkers may see their blood pressure return to normal levels.
What happens on day 4 of no alcohol?
By day 4 of sobriety, the withdrawal symptoms have passed and your body is now feeling the beneficial effects of not drinking alcohol.
You may notice improvements in eating habits, increased water consumption, more physical activity, and better quality sleep.
What factors can influence an individual’s alcohol withdrawal timeline?
Age, gender, genetics, overall health and alcohol use history can all influence an individual’s alcohol withdrawal timeline.
What are the potential medical complications associated with delirium tremens?
Delirium can result in potentially fatal medical conditions, such as cardiac arrhythmia, respiratory arrest, oversedation, or aspiration pneumonitis.
These conditions can be life-threatening and require immediate medical attention. Treatment for delirium symptoms typically includes benzodiazepines to reduce the severity of symptoms, as well as supportive care such as hydration and nutrition. In some cases, medications such as morphine can be dangerous.
What medications are commonly prescribed for treating and preventing severe withdrawal symptoms?
Benzodiazepines are commonly prescribed for treating and preventing severe withdrawal symptoms, such as diazepam, chlordiazepoxide, and lorazepam.
The post A Comprehensive Guide to Alcohol Withdrawal Timeline appeared first on Lantana Recovery: Addiction Treatment Rehab Center.
source https://lantanarecovery.com/alcohol-withdrawal-timeline/
No comments:
Post a Comment